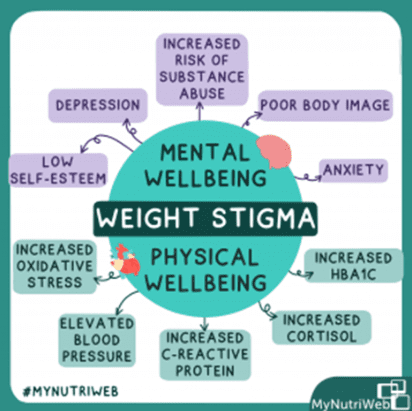
“Weight stigma refers to the discriminatory acts and ideologies targeted towards individuals because of their weight and size. Weight stigma is a result of weight bias. Weight bias refers to the negative” [1]
For the past decade(s) we have heard the ongoing mantra of the ‘Obesity epidemic’ ‘fighting obesity’ or ‘tackling obesity ‘coming from government institutions, the health care industry, Professional organisations, fitness professionals, the field of nutrition and dietetics, and many others. Not to mention the number of profiteering businesses across the health and beauty industry that have used this narrative to market beauty ideals that are mostly unobtainable. This has resulted in health inequalities that have reached a peak, where we can safely say that ‘diet culture’ and weight-centric care are impacting the mental health of individuals across society, resulting in a lack of preventative care, and eventually creating worse outcomes for people seeking healthcare.
There is an ongoing stigmatising narrative aimed at people with larger bodies such as ‘weak willed’ ‘lack self-discipline’, ‘no willpower’, ‘lazy’ that insinuate that living in a larger body is a choice, a direct result of actions of an individual, that it was/is within their control, resulting in an attitude of blame and shame across society at large. What research has shown is that people who suffer from this stigma in their daily life, or experience stigma directly from their health care provider may eventually avoid proper access to healthcare, weaken their health behaviours due to psychological barriers, not receive preventative care, have decreased physical activity, gain more weight, cause disordered eating, and even further develop chronic eating disorders.
There is a call to action for the health care industry to step up, remove the weight stigma paradigm and provide more weight-inclusive care, advocating that we do not strive for a population of thin people, or act to rid society of larger people but collectively work together for a population of ‘healthy people’. There needs to be an acknowledgment that bodies are of diverse sizes and shapes, and that body weight regulation is influenced by multiple factors such as genetic, biological, psychological, social, environmental, and economic where there is a lack of access to nutritious foods. Therefore, weight loss itself should not be prescribed as a clinical outcome, not be measured, or used as a treatment goal. However, there needs to be a safe passage for those wanting to discuss weight and its management who desire to change it. Approaching it through the lens of mindfulness and self-awareness.
The research is ongoing, and studies are demonstrating that weight is not a single cause of poor health outcomes. During the recent nutriweb [2] weight stigma in health care round table discussion, Dr. Angela Meadows [2] presented some fascinating data on there is little or no evidence that suggests weight loss improves overall health and that targeting weight loss as a clinical goal is making people unhealthier. The studies show that healthy habits and managing stress have the biggest influence on health outcomes over loss of weight. She also discussed how healthier living looks the same for people at all BMIs as a person’s BMI is irrelevant if their health habits are poor and vice versa. In addition, she also presented that people who work on body image and body acceptance also prove to have better outcomes over time rather than focusing on weight loss as a health goal. In a study published by Matheson et al the findings explicitly state that “Healthy lifestyle habits are associated with a significant decrease in mortality regardless of baseline body mass index” [3].
For many nutrition professionals, a weight-inclusive approach may be contradictory to what they were taught. We must ask is nutritionist education rooted in a weight-centric paradigm of health? Do nutritionists use language that might unintentionally communicate bias to their clients? What can nutrition professionals do to be role models and advocates for health at every size approach® (HAES) and work with health professionals to raise more awareness? What can nutrition courses include in the curriculum to reflect the current evidence around weight stigma and more weight-inclusive approaches for clients? Nutriri founder Helen James [2] spoke about some nutrition professionals have negative attitudes due to diet culture, but they play a central role in providing care to people with a lived experience of obesity the care should be called nutrition management or health management and get rid of WEIGHT management.
There is a rising cohort of nutrition professionals who are focusing their practice on weight neutrality, weight inclusivity, and incorporating the health at every size approach® [4]. Nutritionists are compassionate towards the lived experiences of others, operating through an anti-oppressive lens that embraces intersectionality. Body Image healing is a route for people to explore their health, body, and food issues deeper and with long-lasting healing in mind. It is often not just one aspect of health that clients are often tackling, there are multiple issues ongoing that can be overwhelming, and a one size fits all approach is not helpful.
When I studied nutrition, I knew deep down that there was something missing. Everything was so prescriptive and un personalised and I intuitively felt people required deeper work to resolve some of their issues around food before they could get to a place where real change occurred. I was drawn to mindful eating as it seemed to be the missing link! But still mindful eating practices alone are not enough for individuals to get to the heart of their body, mind, and food qualms.
Since I have become a nutritional therapist, I have really focused on understanding the psychology of eating to be able to support clients with building the right relationship with food and the body so they can feel nourished and in a better place to achieve good health.
Some of the areas I have trained/training in are Mindful Eating Conscious Living (ME-CL) by Jan Cozen Bay and Char Wilkins. Mindful Based Eating Awareness (MB-EAT) by Andrea Lieberstein. Well Nourished Coaching by Andrea Lieberstein. Emotion Eating and retraining the appetite by Dr. Helen McCarthy. A new course I will undertake is Body Image Training – the missing piece of whole-body healing by Marci Evans. My future study will be around eating nutrition counseling for eating disorders.
This type of work cannot be done in one session and is delivered across multiple sessions, some people chose to continue the work for as long as it takes!
As a nutritional therapist I am committed to creating a safe space for people to deliver nutrition counselling and body image therapy to suit individual needs.
“Until we learn to know ourselves, we should close our eyes and look for a new ways.”
― Santosh Kumar (San)
| [1] W. O. Federation, “our-policy-priorities/weight-stigmas associated with obesity,” 2022. [Online]. Available: ideologiehttps://www.worldobesity.org/what-we-do/our-policy-priorities/weight-stigmas associated with obesity. [Accessed September 2022]. |
| [2] J. Kellow, “understanding-weight-stigma-and-how-to-combat-it,” 07 March 2022. [Online]. Available: https://mynutriweb.com/understanding-weight-stigma-and-how-to-combat-it/. [Accessed September 2022]. |
| [3] nutriweb, “addressing-weight-stigma-in-healthcare,” September 2022. [Online]. Available: https://mynutriweb.com/addressing-weight-stigma-in-healthcare/. |
| [4] “Healthy lifestyle habits and mortality in overweight and obese individuals,” Journal of American board of family medicine , vol. 1, pp. 9-15, 2012. |
| [5] ASDAH, “health-at-every-size-haes-approach,” 2020. [Online]. Available: https://asdah.org/health-at-every-size-haes-approach/. [Accessed September 2022]. |





Comments +